Your Brain After 55: What Nobody Tells You About Cognitive Decline
From risk reduction strategies to tech solutions that actually work
Let’s be honest about your brain: it’s aging, and that comes with real risks. After 55, your chances of cognitive decline start climbing, and by 75, you’re looking at over a 50% lifetime risk of developing dementia. That’s a sobering statistic, but it’s not the whole story.
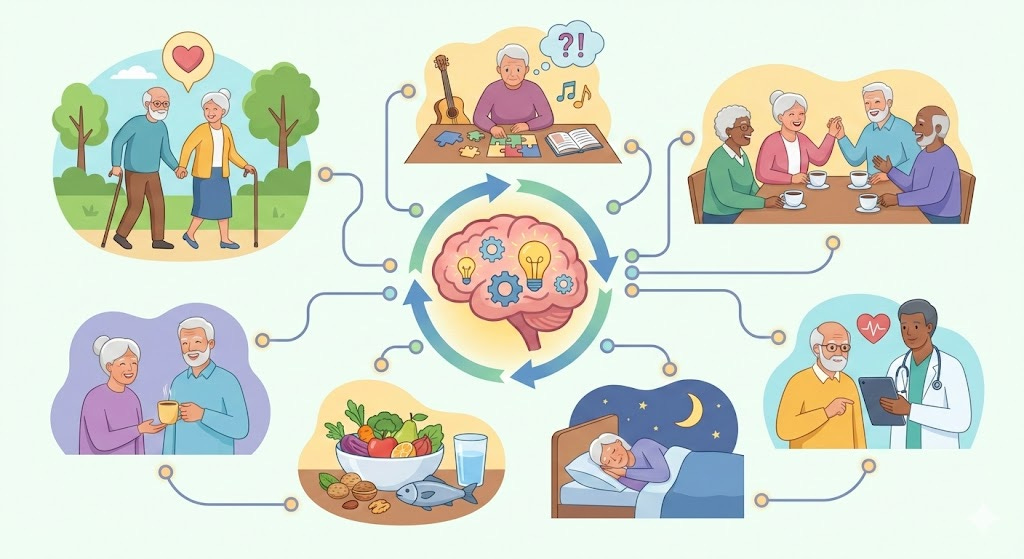
Here’s what makes a difference. Your brain isn’t a static organ that just slowly winds down. It’s remarkably adaptable and responds to what you do with it. The real question isn’t whether your brain will change as you age. It’s whether you’ll take action to keep it healthy while you still can.
Brain Health Requires More Than Puzzles
You’ve probably heard the advice about doing crosswords and staying mentally active. That’s not bad advice, but it’s incomplete. Your brain needs structured workouts, not just occasional stretching. Research shows you need at least 52 hours of combined cognitive or physical exercise to see real, measurable improvements in brain function.
That might sound like a lot, but it breaks down to just one hour per week for a year. The catch is that not all brain activities are created equal. Playing games on your phone won’t get you there. You need targeted training that genuinely challenges your neural pathways.
This is where modern technology finally catches up to the problem. For years, doctors told us to “stay active” without giving us any way to measure progress. Those days are over.
Join our mission to make tech less intimidating for our generation.
Tracking Your Brain Age With Real Data
Thinkie isn’t just another brain-training app making vague promises. It’s a sensor-based system backed by research from NeU Corporation, showing that users can reduce their brain age by an average of 3.7 years after just three months of use. We’re talking about measurable cognitive speed improvements tracked over three years with 178 participants aged 40 to 90.
The long-term users saw even better results, with brain age reductions of up to 10 years after consistent use. The system was designed by Dr. Kawashima, who created the original brain age model. He recommends just 10 to 15 minutes per session, at least twice a week.
What makes a sensor-based system valuable is accountability. You’re not guessing whether today’s mental exercise actually did anything. You have data showing whether your brain is responding to the training.
When Prevention Isn’t an Option
This is where the conversation gets tougher. Maybe you’re reading this and thinking about someone you love who’s already showing signs of memory loss. Or maybe you’re the one who keeps losing track of things, and it’s starting to worry you.
Dementia cases in the United States are expected to double by 2060, reaching one million new cases every year. If you’re 55 or older right now, your lifetime risk of developing dementia is 42%, and researchers say previous studies actually underestimated the real numbers.
Traditional dementia care has been pretty disappointing. We medicate people when they get agitated. We put them in front of regular TV that doesn’t engage them. We watch them decline and tell ourselves there’s nothing more we can do.
But what if there’s a better approach that doesn’t rely on heavy medication?
Music That Actually Works as Therapy
LUCID’s Resonance Rx is taking a different path. This isn’t about playing your favorite oldies in the background. It’s an AI-powered music therapy app that uses facial mapping software to determine how patients respond to specific songs in real time. Then the AI adapts, creating personalized playlists designed to reduce anxiety and agitation in people living with dementia.
The science here is solid. Research has shown that personally meaningful music can reduce agitation, anxiety, and other neuropsychiatric symptoms associated with Alzheimer’s disease. Dr. Frank Russo, LUCID’s Chief Science Officer, notes that these reductions may help decrease reliance on off-label medication use, which has become far too common in care facilities.
What matters most is that this is prescribable. It’s not a wellness trend. It’s a legitimate therapeutic tool that clinicians can use as part of dementia care, helping people maintain more independence and reducing those difficult episodes of confusion and distress.
Television Designed for Dementia
Let’s talk about Zinnia TV. Most television content overwhelms people with cognitive impairment. The quick cuts, complex storylines, loud commercials. It’s sensory chaos when your brain can’t process information like it used to.
Zinnia takes a completely different approach. It’s a streaming service specifically designed with therapeutic videos that are digestible and engaging for people living with dementia. Caregivers use it as a tool to reduce agitation, ease daily activities, and help their loved ones find engagement and connection.
The results speak for themselves: 83% of caregivers say it entertains the person they support, 74% report it reduces agitation, and 79% say Zinnia reduces their own stress as caregivers. That last number matters more than you might think. Caregiver burnout is a real problem, and anything that provides respite while actually benefiting the person with dementia is worth paying attention to.
The Uncomfortable Truth
There’s no cure for Alzheimer’s or most forms of dementia. The research on prevention through lifestyle changes is “encouraging but inconclusive”. Physical activity, blood pressure control, and cognitive training show promise, but they can’t guarantee protection.
That’s uncomfortable to hear. We want certainty and clear answers. But that’s not where we are with brain health.
What we do have is risk reduction. Managing high blood pressure in midlife reduces your risk of cognitive decline later. Staying physically active (at least 150 minutes per week) helps prevent or delay dementia. Preventing or managing type 2 diabetes through diet and exercise makes a measurable difference. Eating a Mediterranean diet focused on vegetables, fish, nuts, and olive oil has been linked to lower dementia risk.
And for those already facing cognitive decline, we now have technology-based tools that genuinely help. They’re not magic solutions, but they’re real interventions that improve quality of life and preserve dignity.
What This Means for You
Your brain health matters. It’s the difference between staying in your own home at 80 or needing round-the-clock care. It’s the difference between recognizing your grandchildren and living in confusion.
You’ve spent your whole life building things, working hard, raising families. Don’t assume there’s nothing you can do about your cognitive health now. Whether it’s using a brain-training sensor like Thinkie to actively improve your cognitive speed, leveraging AI-powered music therapy through Resonance Rx if dementia becomes part of your life, or providing better care through specialized content like Zinnia TV, the tools exist today.
The question is whether you’ll use them before you need them. Or at least know they’re available when that day comes.