Remote Patient Monitoring for Seniors
Why your thermometer suddenly matters more than you think
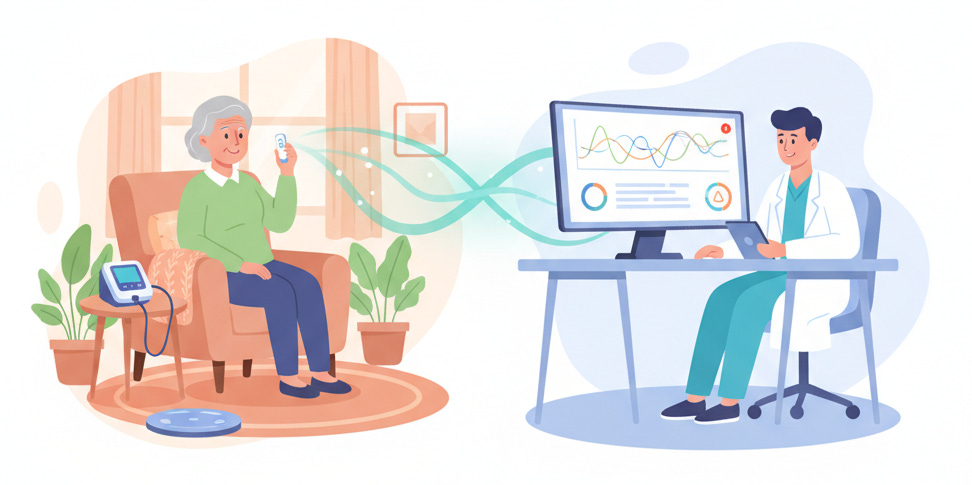
Remote patient monitoring, or RPM, is healthcare that comes to you instead of dragging you into the clinic. It uses everyday medical gadgets in your home to quietly send information to your doctor so problems can be caught early, not after a crisis.
For seniors, that often means devices like blood pressure cuffs, glucose meters, scales, and increasingly, thermometers that send readings automatically over secure networks. The goal is simple: fewer surprises, fewer emergencies, and fewer “why didn’t anyone catch this sooner?” moments.
Why RPM Exists At All
RPM exists because the old way of doing things leaves giant holes in your care. You see your doctor for 15 minutes, then you disappear again for 3 or 6 months while your body does whatever it’s going to do.
During that time, blood pressure can creep up, infections can smolder, and medications can quietly misbehave. By the time something feels bad enough to notice, you might already be heading toward the ER. Hospitals spend billions dealing with these avoidable emergencies in seniors alone.
Remote patient monitoring fills that gap. Instead of relying only on how you feel, your doctor gets a steady stream of real numbers from your home. That stream of data can reduce hospital readmissions for older adults by as much as 40 percent when done properly.
Help other seniors learn about technology that benefits their health by supporting TheSeniorTechie.
So What Actually Happens With Your Data?
Here is the part most people never hear: your doctor is not sitting there staring at a screen waiting for your temperature. No one has time for that. The system watches for them.
RPM systems use rules and alerts. Your care team sets thresholds, like “call us if Mrs. Jones’ temperature goes above 100.4” or “flag any sudden spike over her usual baseline.” The software checks each new reading against those rules and only shouts when something looks off.
Some clinics have staff whose job is to watch those dashboards: nurses or care coordinators who see a list of patients and color-coded alerts. Green is fine, yellow means watch, red means “call now.” That’s how your doctor ends up looking at your temperature in time, without scrolling through every single reading.
What Makes The Doctor Look?
Once your temperature is taken and transmitted, three main things cause a timely response. These are baked into how RPM programs are designed, especially for Medicare patients.
Automatic alerts
If your temperature crosses a preset threshold, the system generates an alert inside your doctor’s monitoring dashboard. It might also send a text, pop-up, or task to the nurse. Abnormal values float to the top of the list so they get attention first.
The system can flag patterns too. For example, a series of slightly elevated temperatures over several days can trigger a “trend alert” even if each reading by itself looks borderline.
Daily review routines
Medicare pays practices specifically to review RPM data each month, with time-based billing codes tied to minutes spent reviewing and reacting to readings. That means clinics build RPM review into their daily workflow, not as an afterthought.
Many programs assign a nurse or care manager to log in at scheduled times each day, check any alerts that fired, and escalate anything serious to the doctor immediately. You are not relying on someone “happening to notice” your data.
Care pathways tied to certain readings
Practices often create simple “if this, then that” plans ahead of time. For example: “If temperature is above 100.4 and the patient has a chronic condition or post-surgery tag, call within one hour and notify the provider.”
These pathways turn a number on a screen into an action: a call, a video visit, a prescription adjustment, or sometimes instructions to go straight to urgent care or the ER.
So your doctor looks in a timely manner because the system insists on it: it flags unusual readings, puts them at the top of the workflow, and ties them to clear next steps. Your one temperature reading does not sit alone in a pile. It joins a living stream of data that the clinic is paid and organized to review.
Why Temperature Is A Bigger Deal In Seniors
Temperature seems simple, but in older adults it is sneaky. Baseline temperatures often run lower, and classic “high fevers” may never appear even with serious infections. A small bump in temperature can mean more in a 78-year-old than in a 28-year-old.
Studies using continuous or frequent temperature monitoring in seniors have shown that fevers are often missed with occasional spot checks alone. In one study, wearable temperature monitoring detected fevers in several older participants that standard care never picked up.
That matters for things like urinary tract infections, pneumonia, and post-surgical complications. Early detection can mean a simple outpatient antibiotic instead of a hospital admission. For people with heart failure, COPD, or diabetes, catching an infection early also prevents those conditions from spiraling.
Where iDigiTemp Fits In
Now the bridge back to that “boring” thermometer on your bathroom shelf. Smart Meter’s iDigiTemp is a forehead and ear thermometer that sends readings over a built-in cellular connection, not WiFi or Bluetooth. It connects automatically to a secure medical network used by clinics for RPM.
There is no app to install, no pairing, no router to reset. You press a button, get a one-second reading, and the device quietly forwards that number through Smart Meter’s cellular platform straight into your provider’s RPM dashboard. That same dashboard is where those alerts, color codes, and workflows live.
The device uses a multi-carrier SIM, which means it hunts for the strongest available cellular network in your area and latches onto it. That is especially useful for seniors in rural areas or in homes with poor internet access, where traditional Bluetooth plus app models often fail completely.
Why Doctors Actually Notice iDigiTemp Readings
Because iDigiTemp integrates into existing RPM platforms, your temperature data shows up in the same place as your blood pressure and glucose readings instead of in some separate app no one checks. The same alert rules are applied: thresholds, trends, and flags.
Smart Meter’s platform is already used for hundreds of thousands of patients in remote monitoring programs. Clinics using that platform can simply add temperature as another vital sign to track. When your reading crosses the line they set, it surfaces on their daily RPM review list.
In practical terms, this means:
You take the reading.
The thermometer sends it automatically through the cellular network.
The RPM system compares it to your personalized thresholds and recent history.
If it looks concerning, the system pushes your case into view for the nurse or care manager that day, often with a red or urgent status.
That is what causes a timely look. Not hope. Not chance. A system designed so your data knocks on the clinic’s door when it needs attention.
The Problem This Solves, And The Real Solution
The core problem for seniors is dangerous silence between appointments: subtle changes go unnoticed until they become big, expensive, and scary. Traditional thermometers keep that silence because the only person who sees the number is you, and you may not know when it matters.
Remote patient monitoring breaks that silence by streaming vital signs to your healthcare team in small, regular pieces. Smart Meter’s iDigiTemp solves the last mile of that system for temperature: it removes the tech headaches that kept many older adults from participating and plugs each reading into alert-driven workflows that force timely review.
The solution is not “buy a fancy gadget.” The solution is enrolling in an RPM program with your doctor where your readings, including temperature, are tied to clear rules and responses. In that setting, a simple one-second thermometer reading can be the event that triggers a nurse’s phone call before you ever feel “sick enough” to call them first.